Erythrocyte sedimentation rate as a marker for coronary heart disease
Yayan J.
Vascular Health and Risk Management, 2012
Determination of the erythrocyte sedimentation rate
is a nonspecific test that constitutes one of the oldest
laboratory methods. An accelerated erythrocyte
sedimentation rate may be indicative of inflammation
or the presence of a tumor. However, a slow erythrocyte
sedimentation rate may occur (e.g., in polycythemia
vera). Despite the critical role of cytokines in inflammatory
conditions, the erythrocyte sedimentation rate still plays
an important role in the diagnosis and follow-up
of rheumatoid arthritis and temporal arthritis, sickle cell
disease, and osteomyelitis, as well as in noninflammatory
conditions such as stroke, coronary artery disease,
and prostate cance.
Patients with symptoms of angina pectoris or myocardial
infarction frequently present without striking evidence
of cardiac-specific enzymes in blood laboratory
assessments or specific electrocardiogram findings.
The purpose of this study was to assess the efficacy
of the erythrocyte sedimentation rate as a potential
additional indicator for coronary heart disease so that
patients with angina pectoris or myocardial infarction can
be more rapidly identified and treated.
This study differs from other studies in that all patients
were examined by coronary angiography with multiple
blood tests and patients with inflammation and tumor
were excluded from this study. This meant that the
erythrocyte sedimentation rate and acute coronary
heart disease could be studied better by close temporal
investigations.
This was a retrospective study of patients with angina pectoris, non-ST-elevation myocardial infarction, or acute myocardial infarction with ST-segment elevation, as assessed by electrocardiography. All patients included in this study underwent coronary angiography, resulting in the diagnosis of acute coronary heart disease. Patients in whom coronary heart disease was excluded by coronary angiography served as controls. The erythrocyte sedimentation rate was measured over a period of 1 hour and 2 hours; normal values were considered to be < 10 mm in the first hour and < 20 mm in the second hour. The number of leukocytes was also determined in all patients; the normal number of leukocytes was considered to be 4.000–10.000 cells/µL. C-reactive protein (CRP) level was determined in all patients, with a normal reference value of, 6.0 mg/L. The average number with standard deviation of neutrophils, lymphocytes, monocytes, eosinophils, and basophils was determined as a percentage of patients with prolonged erythrocyte sedimentation rate and coronary heart disease. Any inflammatory disease was excluded in all patients by clinical and radiologic assessment and by urine sediment or urine culture. Patients with angina pectoris diagnosed with inflammatory or tumor diseases were excluded from the study.
Data are presented as mean ± standard deviation. The χ2 test was used to compare prolonged erythrocyte sedimentation rates between patients with and without coronary heart disease. The specificity and sensitivity of the erythrocyte sedimentation rate as a marker for coronary artery disease and the 95 % confidence interval (CI) were calculated.
A total of 136 patients with angina pectoris or acute myocardial infarction were included in this study (Figure below). The cohort included 89 men and 47 women with an average age of 69.31 ± 12.45 years.
During cardiac catheterization, 102 (75 %) patients were
found to have coronary heart disease, including 70
(68.63 %) males and 32 (31.37%) females. A total of 52
(38.24 %) patients were diagnosed with angina pectoris,
39 (28.67 %) with non-ST-elevation myocardial infarction,
and ten (7.35 %) with acute ST-elevation myocardial
infarction. The indication for coronary angiography was
performed in 35 (25.74 %) patients due to changes
in the electrocardiogram such as negative T, R-regression,
and pathological ergometry. Further, 59 patients had
three-vessel disease, 24 patients had two-vessel disease,
and 19 patients had one-vessel disease. No coronary
heart disease was seen in 34 (25 %) patients, including 19
(55.88 %) men and 15 (44.12 %) women.
The erythrocyte sedimentation rate was prolonged in 79
(58.09 %) patients. Coronary heart disease and a prolonged
erythrocyte sedimentation rate were observed in 69
(50.74 %) patients (95 % CI ± 8.4 %, 42.34 %–59.14 %)
with an average value of 19.68 ± 12.71 mm in the first
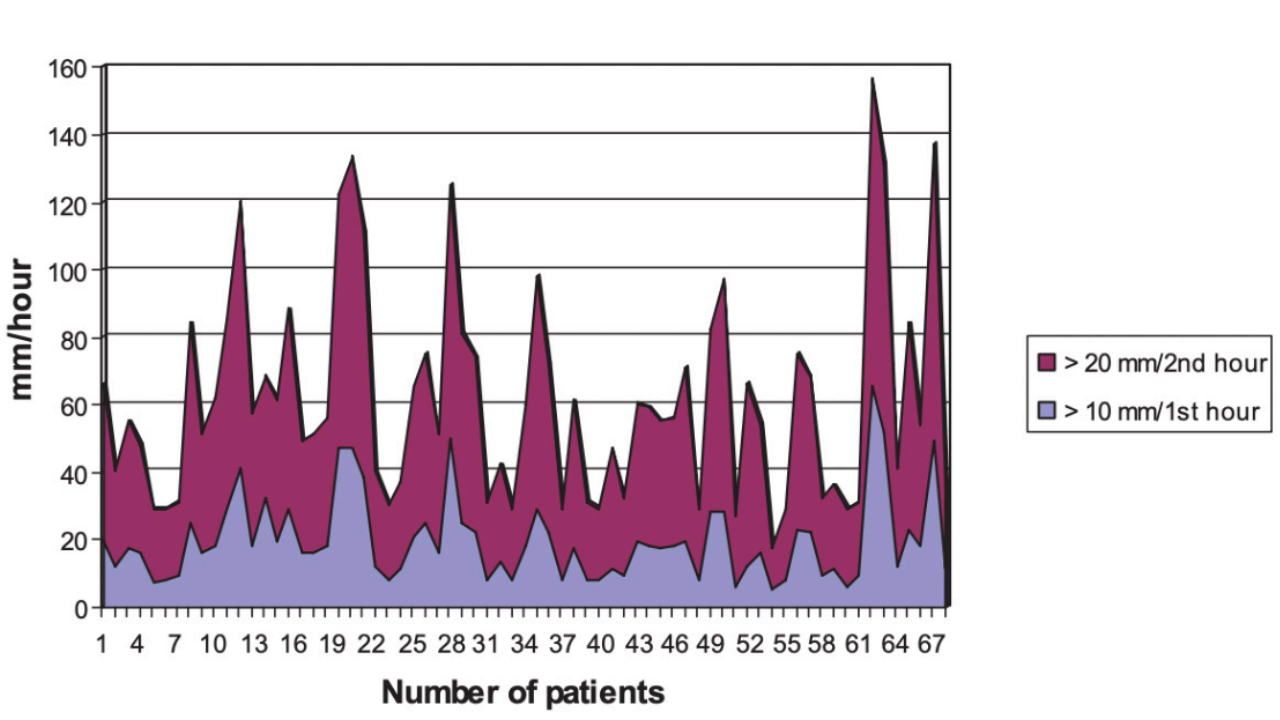
hour and 41.88 ± 19.30 mm in the second hour (Figure below).
The erythrocyte sedimentation rate was prolonged in ten
(7.35 %) patients (95 % CI ± 4.39 %, 2.96 %–11.74 %).without signs of significant stenosis by coronary
angiography. A normal erythrocyte sedimentation rate
was seen in 24 (17.65 %) patients (95 % CI ± 6.41 %,
11.24 %–24.06 %) without evidence of coronary heart
disease by cardiac catheterization. In contrast, 33 (24.26 %)
patients (95 % CI ± 7.2 %, 17.06 %–31.46 %) with a normal
erythrocyte sedimentation rate exhibited signs of ischemic
coronary heart disease by left heart catheterization.
The specificity of the erythrocyte sedimentation rate
for coronary heart disease was 70.59 % and the sensitivity
was 67.65 %. However, the two-sided significance using
the χ2
test was not significant for a prolonged erythrocyte
sedimentation rate being indicative of coronary heart
disease
The average number of leukocytes in all patients was
8.596 cells/µL ± 2.578cells/µL. The average increased
leukocyte value in 35 (25.74%) patients was 12.003 ±
2.108 cells/µL and in 19 (13.97%) patients with coronary
heart disease and prolonged erythrocyte sedimentation rate
12.072 ± 2.183 cells/µL (Figure below).
The average elevated CRP value in 49 (36.03 %) patients was 19.04 ± 20.77 mg/L; in 32 (23.53 %) patients with an acute coronary heart disease and prolonged erythrocyte sedimentation rate 18.67 ± 16.95 mg/L (Figure below).
The average number of neutrophils was 67.14 % ± 11.07 % (reference range 50 %–70 %), 22.04 % ± 9.70 % (20 %–52 %) lymphocytes, 8.75 % ± 2.57 % (3 %–7 %) monocytes, 1.84 % ± 1.28 % (1 %–4 %) eosinophils, and 0.37 % ± 0.22 % (0 %–1 %) basophils. The neutrophils were increased in 27 (39.13 %) patients from a total of 69 patients with coronary heart disease and prolonged erythrocyte sedimentation rate with coronary heart disease.
The findings of this study suggest a possible correlation
between a prolonged erythrocyte sedimentation rate
and coronary heart disease. Indeed, the erythrocyte
sedimentation rate was mostly prolonged in patients
with coronary heart disease. However, although the
specificity and sensitivity of the erythrocyte sedimentation
rate as a marker for coronary heart disease were relatively
high, the χ2
test showed a nonsignificant effect.
Erikksen et al previously reported that the erythrocyte
sedimentation rate may be a good indicator for coronary
heart disease, mortality, and the risk of death from coronary
heart disease. The relationship between the erythrocyte
sedimentation rate and the risk of coronary heart disease
was also assessed in a cohort study by Andresdottir et al.
The authors concluded that the erythrocyte sedimentation
rate can be used as an independent prognostic factor
for coronary heart disease in men and women on the basis
of an inflammatory process of atherosclerosis However,
it has been shown that the erythrocyte sedimentation rate
cannot be used for screening and check-up examinations
in asymptomatic patients. Nevertheless, Gillum et al
described that an increased erythrocyte sedimentation rate
is a risk factor for coronary heart disease. This relationship
between the erythrocyte sedimentation rate and the risk
of coronary heart disease was also observed in this study.
The other inflammatory parameters were also elevated
in this study. Therefore, this assumption of inflammation
as a basis for the development of atherosclerosis was also
confirmed through this recent study.
A relationship between coronary atherosclerosis and
erythrocyte sedimentation rate was found in a clinical
observation study by Natali et al. In the present
study, seven patients were diagnosed with coronary
atherosclerosis by cardiac catheterization. In three cases
of arteriosclerosis, the erythrocyte sedimentation rate was
extended in this study.
Serum levels of myocardial enzymes and inflammatory
biomarkers have been shown not only to be increased
in the setting of an acute coronary event but also
to quantitatively correlate with the extent of myocardial
damage and coronary artery disease severity, according
to angiographic findings CRP is the most widely
studied inflammatory marker, and there is now robust
evidence that CRP is a strong predictor of cardiovascular
risk among apparently healthy individuals, patients
undergoing elective revascularization procedures,
and patients presenting with acute coronary syndromes. Circulating levels of CRP rise during the acutephase response to tissue injury, infection, and inflammation, and CRP, the prototypic acute-phase protein, and
to a lesser extent fibrinogen, have been proven to be
reliable and important markers of the risk of ischemic heart
disease. Also in this study, elevated levels of CRP were
observed in about one third of patients with acute coronary
heart disease after exclusion of inflammation.
A correlation has also been observed between leukocyte
count and acute coronary syndrome; investigations
of the utility of the leukocyte count as a risk factor and
prognostic indicator in patients with acute coronary
syndrome are consistent with the current concept that
atherosclerosis is an inflammatory disease.
Leukocytosis induces or worsens coronary heart disease
through multiple pathologic mechanisms that mediate
inflammation, cause proteolytic and oxidative damage
to endothelial cells, plug the microvasculature, induce
hypercoagulability, and promote infarct expansion.
In summary, it has been consistently shown that
leukocytosis is an independent risk factor and prognostic
indicator of future cardiovascular outcomes, regardless
of disease status. The leukocyte count is inexpensive
to obtain, reliable, easy to interpret, and ordered routinely
in inpatient and outpatient settings. Also in this study,
leukocyte counts in all patients with acute coronary
heart disease were increased, on average. Therefore,
a relationship between leukocyte account and acute
coronary heart disease has also been observed in this
study.
The independent association of neutrophil count with the
angiographic characteristics of coronary atherosclerosis
strongly suggests that granulocytosis may play a role
in the development of coronary atherosclerosis.
The granulocytes from patients with prolonged erythrocyte
sedimentation rate with coronary heart disease in this study
were not increased, on average, apart from individual
elevated values.
The erythrocyte sedimentation rate was found to be frequently prolonged in patients with coronary heart disease. An increase in erythrocyte sedimentation rate provides information about the inflammatory etiology of coronary heart disease. The erythrocyte sedimentation rate may thus be helpful as an additional diagnostic tool for coronary heart disease.
© 2024 West Medica. Все права защищены
Любая информация, содержащаяся на настоящем сайте, носит исключительно справочный характер, предназначена для информационных целей и ни при каких обстоятельствах не может быть расценена как предложение заключить договор (публичная оферта). West Medica не дает гарантий по поводу своевременности, точности и полноты информации на веб-сайте, а также по поводу беспрепятственного доступа к нему в любое время. Спецификация и технические характеристики продуктов, их изображение, условия приобретения, цены, спецпредложения и комплектации, указанные на сайте, приведены для примера и могут быть изменены в любое время без предварительного уведомления. Для получения более точной и подробной информации, необходимо обращаться к сотрудникам компании.